The Importance of EHR Migration
Electronic Health Records (EHR) Migration is the process of transferring patient data, clinical workflows and system configurations from one EHR platform to another. In 2025, health organizations quickly migrate to increase interoperability, improve patient care and follow the rules that develop. Global EHR is estimated to reach $ 47 billion by 2027 with the market, according to Fortune Business Insights, migration is inspired by the need for advanced features such as AI analysis, cloud-based access and patient engagement tools. Successful migration data ensures integrity, reduces disruptions and provides the supplier to positions for long -term efficiency and innovation.
Why Healthcare Organizations Migrate EHR Systems
EHR migrations are inspired by many factors. Heritage systems often lack interoperability by preventing the data sharing required by regulations such as the 21st century Treatment Act. Modern platforms, such as Epos or Sarners, provide advanced functionality, including telehaalth integration and future indication analysis, improving clinical results. Cost reduction is another driver, as cloud-based EHRs such as Athanhealth Low Maintenance Expenses 20%, according to Klas Research. The merger and procurement require integrated systems, while the user’s dissatisfaction indicates the switch with the old interface. In 2025, 60% of the 60% health care provider reflects the EHR upgrade plan, according to Black Book Market Research, increased efficiency and pushing patient-focused care.
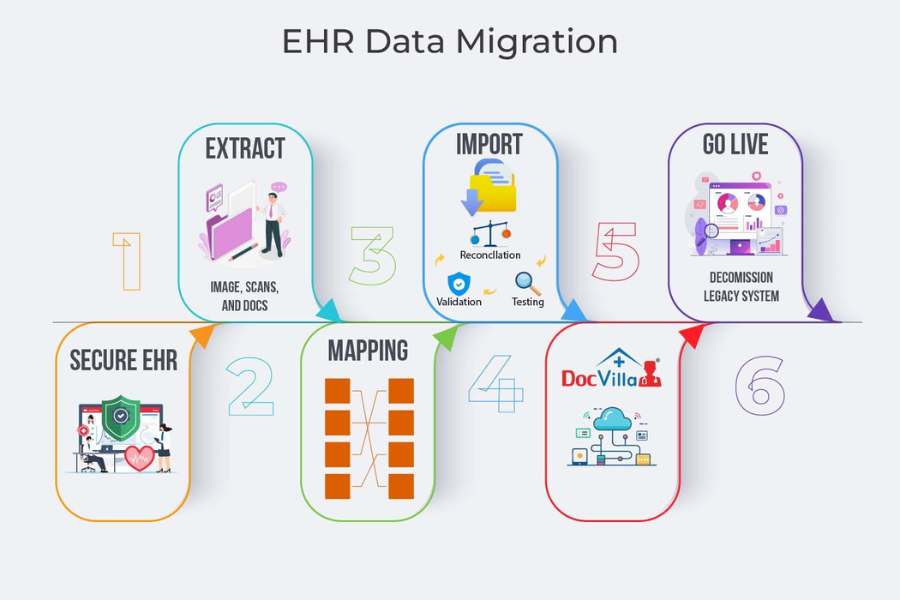
Key Steps in the EHR Migration Process
A structured EHR migration process is important to succeed. Planning begins with defense of the goals, such as improving interoperability or reducing costs, and collecting a multi -from -team of doctors, IT employees and administrators. The data assessment identifies the items to migrate and ensure compliance with hipa. Mapping and cleaning the data using a tool such as Redox Standardize the formats for accuracy. System selection involves evaluating platforms such as Allscripts or NextGen for compatibility. The test validates the workflakes, while training prepares employees through platforms such as Healthstreams. The Go-Laive is phased out to reduce disturbances, followed by migration support to solve questions. This methodological approach ensures a smooth transition.
Challenges in EHR Migration
EHR migrations present important challenges. Data integrity occurs during transmission, where 30% of migration faces loss of data or corruption, Per HIMS. Differences between inheritance and new systems complicate mapping, especially for non-standard forms. Staff’s resistance, motivated by changes in the workflow, affects the adoption, with 40% of doctors, reporting burnout during infection, during medscape per medscape. High costs, intermediate size, on average $ 500,000 to $ 1 million for stress budget. During Go-Live, downtime may interfere with the patient’s care, while CMS adds regulatory compliance, including the rules of interpretation. In order to cope with these challenges, a strong plan, dedication and specialist support are needed.
Technologies Supporting EHR Migration
Advanced technologies streamlining EHR migration in 2025. Cloud-based platforms such as Amazon Web Services (AWS) provide scalable data storage and secure transfer, reducing costs by 25%. AI-driven equipment, such as innovate, automate data resort and mapping, improves accuracy up to 90%. Interoperability standard, such as FHIR (Fast Healthcare Interoperability Resources), supports the seamless data exchange, supported by the Redox API. Blockchain used by platforms such as Healthchain, which ensures HIPAA compliance, increases data security during migration. The robot process introduced by Uipath automatically stores repetitive features such as patient updates saves hours. These technologies increase the efficiency and reliability of the migration process.
Best Practices for Successful EHR Migration
It is necessary to use the best practice for a spontaneous EHR migration. Attach early stakeholders, including doctors and patients to coordinate the goals and reduce the resistance. By using devices such as Varato for identity matching, you perform a complete data audit to ensure perfection. The pilot test with a small dataset, as recommended by ONC, validates system functionality before full migration. To promote the trust of the employees, you can take advantage of e-learning platforms such as Dosbo, provide extensive training. Use a phase Go-Live, which starts with non-comrades, to reduce disorders. Maintain strong communication through devices such as slack to remove real -time concerns. These practices ensure data integrity, users use and operational continuity.
The Role of Vendor and Consultant Support
EHR sellers and advisors play an important role in migration. Sellers such as Epic and Meditech provide migration tool sets including data recovery templates and interoperability -Py -er, streamlining transitions. People of Deloite or Tagria, such as project management, who specialize in data mapping and compliance, reduce the risk per 50%per gardener. They evaluate speed, adapt the workflow and mediate among the stakeholders. For example, Carner’s migration services include the support dedicated to the Go-Live steps. Listed in Kla’s Research Rankings, selection of suppliers with a perfect track record, ensures reliable partnerships, migration increases the success and performance of long -term systems.
Impact on Patient Care and Outcomes
EHR migration, when effectively performed, the patient’s care significantly increases. Modern systems improve data access, allowing doctors to make informed decisions, after better results by 70%, migration, Per Hims. Integrated into platforms such as patient portal, ethhaneth, increase engagement, patients with 40% patients who reach online posts in 2025, per onc per onc. The future analysis available in the EPIC platform identifies risk patients and reduces reduction by up to 15%. However, poorly controlled migration can disrupt care, 20% of suppliers are reported to be delayed during infection. Preference to minimal shutdown and strong exercise ensures migration to translate into better clinical efficiency and patient satisfaction.
Cost and Time Considerations
EHR migations are resource-intensive, costs and deadlines differ from the size of the outfit. Little practice can cost $ 100,000- $ 500,000, while large hospitals over $ 10 million, according to Health Care News. Large expenses include software licenses, upgrade fee for hardware and counseling. Timeboundy varies from 6 months to small clinics for hospitals for 2 years, with computer and training 60% plan. Cloud -based solutions reduce the cost of re -eliminating infrastructure, while phased approaches reduce abbreviated shutdowns. Budget for migration support, including adaptation, ensures that long -lasting ROI, with 80% of suppliers, within 3 years, reinforces the costs of the black book.
Future Trends in EHR Migration
By 2025, the Migration of EHR is a strategic requirement for health organizations that require differences, patient care and an increase in efficiency. To ensure migration utilization technologies such as AI, Cloud Computing and FHIR data integrity and streamlined procedures to ensure regulatory mandate and streamlined procedures run by cultural men’s systems. Regardless of high costs and resistance from employees, the best practice in the form of engagement, faced lotus life and strong exercise, risk. Sellers, including automation and patient fishing functions, increase further and new trends, success. By demonstrating well induced migration, suppliers can unlock advanced EHR skills, provide better results and a permanent, in the health care system to give itself a position for innovative future.
Conclusion
By 2025, EHR migration is a strategic requirement for health organizations that require increasing interoperability, patient care and efficiency. Migration utilization technologies such as AI, Cloud Computing and FHIR to ensure data integrity and streamlined processes driven by the boundaries of regulatory mandate and cultural men’s systems. Despite high costs and resistance from employees, best practices as commitment, phased cumel life and strong training, the risk. Sellers, including automation and patient -focused functions, increase support further and new trends, success. By performing well -planned migrations, suppliers can unlock advanced EHR skills, provide better results and position themselves for a permanent, innovative future in the health care system.